The collateral effects of COVID-19
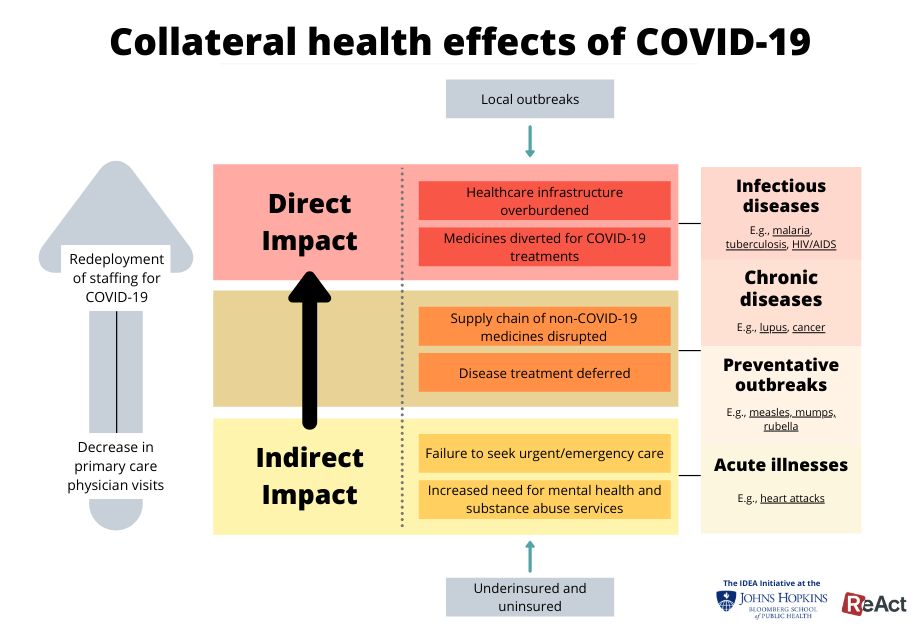
The COVID-19 pandemic has strained the healthcare delivery system. Apart from caring for COVID-19 patients, this has resulted in both direct and indirect collateral effects on health care. Local outbreaks have exacerbated underlying health inequities, particularly among the underinsured and uninsured. And the uninsured and underinsured, particularly in the U.S. healthcare delivery system, magnify the problem by failing to seek care for suspected COVID-19.
COVID-19 collateral health effects
Many potential treatments for COVID-19 seek to repurpose drugs now being used in caring for other patients. This has resulted in the diversion of these medicines from meeting the needs of non-COVID-19 patients and has contributed to both price hikes and shortages. While much of the lock-down and social distancing measures have worked to “flatten the curve,” the healthcare delivery system has become burdened in key ways: 1) by the surge capacity built up to meet the influx of new COVID-19 patients; and 2) by system-wide effects as primary care visits fall and staff are redeployed to wards set up for COVID-19 patients.
Non-COVID-19 collateral health effects
Beyond the COVID-19 collateral health effects, however, the ongoing pandemic has had broader impact. Vaccination rates have dropped by more than 70% in some countries, with nearly two dozen countries suspending national immunization programs and GAVI, The Vaccine Alliance suspending another 14 immunization campaigns. All together, the Measles & Rubella Initiative (M&RI) estimates that more than 117 million children across 37 million countries may miss out on receiving the measles vaccine. Meanwhile, GAVI’s suspension of immunization programs alone has already affected more than 13 million people in 13 of the world’s least-developed countries. History reveals that the collateral health impact can exact a significant toll as well. Between 2013 and 2016, a decrease in vaccination numbers attributable to the Ebola epidemic led to outbreaks of measles that killed more people than Ebola itself. As COVID-19 continues to overburden the global healthcare system, local preventative outbreaks will only continue to increase both the human and financial toll.
In addition to depressed vaccination rates, however, COVID-19 has disrupted the medicines supply chain, putting dozens of pharmaceutical products at risk. While 40% of active pharmaceutical ingredients (APIs) for generics in the United States are imported from India, the Indian Government recently announced restrictions on 26 different APIs and products, including common drugs such as acyclovir and paracetamol. India had relinquished export restrictions on hydroxychloroquine, an antimalarial drug that some had suggested as a treatment for COVID-19, at the request of the Trump Administration. Meanwhile, China’s drug manufacturing sector is still reeling from COVID-19 shutdowns, causing additional disruptions. In countries such as the United States, these disruptions are already materializing, with the US FDA announcing shortages of pindolol, a drug commonly used for the treatment of hypertension and cardiovascular disease. As funders such as the Global Fund for AIDS, TB and Malaria continue to prioritize COVID-19, at the expense of other treatments, shortages of necessary drugs will only continue to increase globally, especially in developing countries. Indeed, the Bill and Melinda Gates Foundation, the world’s largest charity, recently announced the Foundation would focus on COVID-19—at the risk of its other public health programs suffering.
Disease-specific challenges emerging from collateral health effects
From acute illnesses to chronic diseases, COVID-19 has already had a tangible impact on a variety of diseases. The World Health Organization expects malaria deaths through sub-Saharan Africa to increase by 200%, with deaths projected to reach 769,000, driven by overburdened healthcare infrastructure systems, shortages in medicines and disruptions in the supply chain, as well as diversions of laboratory activities and clinical services. If observed, this increase alone would put the world back 20 years in the fight against malaria. Similarly, this story holds true for a variety of infectious diseases, with tuberculosis deaths in children alone expected to exceed 250,000 and multi-drug resistant tuberculosis posing greater burdens on populations, especially those in low- and middle-income countries.
For chronic diseases, supply chain disruptions and deferred disease treatments are also expected to drive an increase in disease burdens. In Nigeria, for example, the cost of hydroxychloroquine jumped from $5.50 to $34.70 per 30 tablets, making it unaffordable for those that use it for lupus treatment. As a result, up to 60% of lupus patients, the vast majority of whom are women, face shortages in hydroxychloroquine. Hydroxychloroquine plays an important role in controlling complications of lupus during pregnancy, reducing complications and maternal mortality. Meanwhile, overburdened hospitals and physician shortages have increased the challenges in treating chronic diseases such as cancer. As lockdowns are implemented, patients have been forced to take cancer treatment regimens with increased dosages, balancing the risks of potentially greater toxicity and side effects.
Moreover, healthcare systems around the world are seeing decreases in urgent and emergency care for acute illnesses. In the United States, for example, the number of severe heart attacks being treated in hospitals dropped by nearly 40%. At the same time, emergency medical personnel across the country reported a 400% increase in house calls for cardiac symptoms, with the majority of these patients dying at their homes. For other acute illnesses like appendicitis and stroke, the numbers similarly suggest a decrease in emergency and urgent care.
Outside the healthcare delivery system, challenges in the food system and in sustaining the livelihoods of the poor have taken a significant toll. The World Bank projects that as many as 49 million people could be pushed into extreme poverty by the end of 2020 with an estimated 265 million people facing acute food insecurity globally. With unemployment rates hitting record highs and trade falling by as much as 32%, the economic and system-wide effects of COVID-19 are on an upward trajectory. As lockdowns are extended over several months, the need for mental health and substance abuse services have skyrocketed.
But the lockdown has also been accompanied by transient health gains. Blue skies can once again be seen in some cities once covered by air pollution and smog. As a result, in some cities such as China, one environmental economist has estimated that the near-term benefit of reduced pollution over two months translates into the saving of 4000 children under age 5 and 73,000 adults over age 70 in China. While this evidence varies by city, there has also been a decrease in trauma admissions due to lockdown--in some countries, by as much as 43%. As stay-at-home restrictions are lifted in countries around the world, plans to build such health gains sustainably into the new normal have not materialized.
As we work to address the COVID-19 pandemic, there are opportunities not only to advance needed infrastructure to stem the spread of emerging infectious diseases like this, but also to turn back the rising tide of antimicrobial resistance. Such efforts might include addressing zoonotic sources of disease transmission, improving local disease surveillance, enhancing infection prevention and control in healthcare facilities, and ensuring surge capacity to deliver diagnostics, drugs and vaccines. As the response to COVID-19 calls for improved laboratory testing and respiratory support with pulse oximetry, oxygen concentrators and even ventilators, such equipment might be better positioned to reach district hospitals that might once have gone without such infrastructure. The direct harms of this spreading pandemic and the collateral health effects of addressing it make charting an equitable path forward one of the greatest challenges ahead.